
What is Denial Code CO 97? YouTube
When it comes to the 97 CO Denial Code it precisely stands for denial when the products or services cannot be separately paid for. Wondering what this might mean? This signifies that the service of the product has already been covered under some other segment and hence the claim cannot be paid separately.

Remittance explanation codes amerigroup
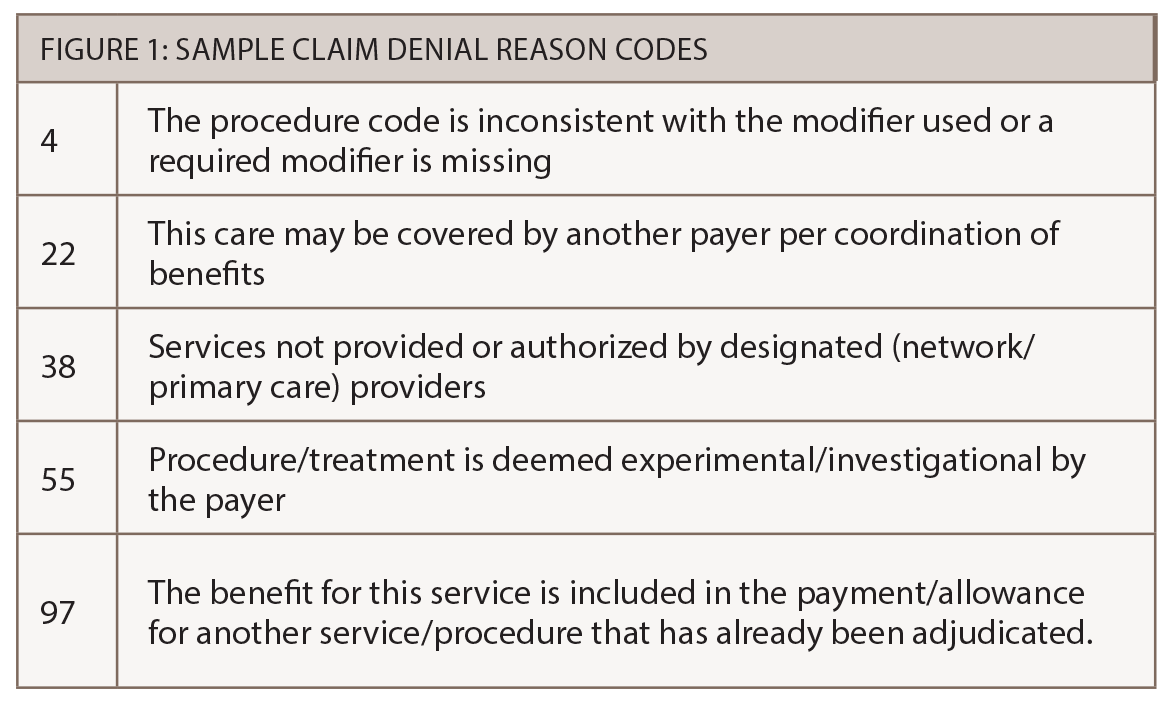
The Fabric of Denial Codes. CO (Contractual Obligations): Denotes contractual agreements between the provider and the insurance payer. For instance, CO 97 implies that the claim was denied because the service is included in another service or procedure already adjudicated.

Medical Billing Forum Medical Billing Process Guide
Denial Code CO 97 occurs because the benefit for the service or procedure is included in the allowance or payment for another procedure or service that has already been adjudicated..

What is CO 22 Denial code in medical billing and how to work on it Bcbsproviderphonenumber
CO-97 indicates the service or procedure billed is not reimbursed separately because payment is considered bundled into the allowance for another service already adjudicated. In plain terms, you won't get paid extra for the denied service because the insurer believes it is included or should be grouped with another service they already reimbursed.

CO 24 Denial Code Charges covered under capitation agreement or managed care plan
Denial reason code CO 97 We received a denial with claim adjustment reason code (CARC) CO 97. What steps can we take to avoid this denial? The benefit for this service is included in the payment/allowance for another service/procedure that has already been adjudicated.

Denial Code CO9 Diagnosis Code is Inconsistent with the Patient’s Age
Channagangaiah November 19, 2020 Insurance deny the claim with CO 97 denial code, when procedure code is inclusive with the other procedure code billed or another service for the same patient that has already been billed and adjudicated. Let us learn some of the following medical terms for decoding the above denial:

What is Denial Reason Code CO 24 and CO 22? How to Resolve Them? Atlantic RCM
These codes describe why a claim or service line was paid differently than it was billed. Did you receive a code from a health plan, such as: PR32 or CO286? If so read About Claim Adjustment Group Codes below. About Claim Adjustment Group Codes Maintenance Request Status Maintenance Request Form 11/1/2023 Filter by code: Reset

Denial Code CO 97 An Ultimate Guide — Etactics
The CO 97 Denial Code plays a crucial role in medical billing, signaling that a service or procedure isn't eligible for separate payment. Essentially, the benefit for a given service or procedure is already included in the payment for another previously adjudicated procedure or service.

Denial Code CO 97 An Ultimate Guide — Etactics
What is Denial Code CO 97? Watch on As a medical coding expert, I'm sure when you submit your claim it always gets accepted. Right? Don't worry, no one is THAT much of an expert. Like I said before, claim denials are a part of the game. Unfortunately, you won't be able to avoid these.

DENIAL CODE CO197 How to Avoid PreAuthorization Denial? MD Billing Facts
View common corrections for reason code CO-97, CO-B20 and RARC N111.

Denial Codes in Medical Billing 2023 Comprehensive Guide
Denial reason code CO 97 FAQ To enable us to present you with customized content that focuses on your area of interest, please select your preferences below: Select which best describes you: Health Care Professional Person (s) with Medicare Select your location: Florida Puerto Rico U.S. Virgin Islands Select your line of business: Part A Part B
CO 24 Denial CodeCharges are covered under a capitation agreement
The denial code is CO-97. Is there anything we can do with these ultrasounds to minimize the denials? Any modifiers that we can use. Thank you in advance for your help. Misty Dawn Guru. Messages 173 Location Spokane, WA Best answers 0. Feb 1, 2018 #2 aridalia said:
4 Steps to Prevent Unnecessary Claims Denials The Rheumatologist
To address denial code CO-97: Check whether the procedure code belongs in the inclusive, exclusive, or bundled category Once you've identified the procedure code type, get in touch with the coding division and inquire as to whether a modifier can be used before resubmitting the claim. Ask the claims department how to file an appeal.

Denial Code CO109 Service Not Covered by this Payer MD Facts
Denial Code CO 97 occurs because the benefit for the service or procedure is included in the allowance or payment for another procedure or service that has already been adjudicated. Basically, the procedure or service is not paid for separately.

Denial Code CO 97 An Ultimate Guide — Etactics
Solutions for Denial Code CO 97: In some cases, there are some solutions for denial Code CO 97 because there are times when services may be billed separately, even if they are usually bundled with another service. Steps to follow include: Start out by checking to see which procedure code is mutually exclusive, included, or bundled.

Denial Code CO 97 An Ultimate Guide — Etactics
CO 97 denial code is not exclusive to capitation-related denials. It is a more general code that signifies a denial based on contractual agreements. Specific codes related to capitation may vary depending on the insurance company's coding system. What Does Denial Code 95 Mean?